Healthcare & Medical

Why System Design Matters More Than Speed
Healthcare and medical organizations operate in environments where execution risk has real human consequences. Delays, misaligned incentives, and weak decision structures do not just affect delivery timelines; they surface later as patient risk, regulatory exposure, clinician burnout, and operational instability.
Most healthcare initiatives do not fail because teams lack expertise or effort. They fail because critical decisions are made inside systems that were never designed to support safe execution under pressure.
This article explains where execution risk concentrates in healthcare, why it is structurally different from other industries, and how organizations can reduce that risk without relying on optimism, heroics, or excessive tooling.
What Is Execution Risk in Healthcare?
Execution risk in healthcare refers to the likelihood that decisions, once made, will produce unintended or harmful outcomes due to system design rather than individual error.
In practice, execution risk increases when:
- Decision ownership is unclear
- Feedback arrives too late to correct course
- Incentives reward short-term output over long-term stability
- Systems depend on specific individuals or vendors
- Compliance requirements shape architecture without considering adaptability
Unlike other industries, healthcare often experiences the consequences of execution risk months or years after decisions are locked in.
Why Healthcare Execution Risk Is Structurally Different
Healthcare and medical organizations face a combination of constraints that amplify execution risk:
Irreversible Decisions
Clinical workflows, data schemas, vendor integrations, and compliance architectures tend to persist for long periods. Reversing them is expensive, disruptive, or impossible.
Distributed Accountability
Responsibility is spread across clinicians, administrators, compliance teams, vendors, and regulators. Without explicit decision ownership, accountability diffuses.
Delayed Feedback Loops
The impact of architectural and process decisions often appears long after implementation, when options for correction are limited.
Regulatory Coupling
Regulatory frameworks define minimum requirements, not resilient system design. Organizations often optimize for audits instead of operational stability.
Human-Critical Workflows
Healthcare systems must support people operating under cognitive load, stress, and time pressure. Small design flaws scale rapidly under real-world conditions.
These factors make healthcare execution risk difficult to detect early and expensive to correct later.
Common Healthcare Failure Modes
Across providers, medical device companies, digital health platforms, and healthcare SaaS organizations, the same execution failures recur:
Vendor Dependency
Platforms are adopted to accelerate progress but gradually constrain decision-making, increase switching costs, and reduce internal capability.
Hero-Based Execution
Outcomes depend on a small number of experienced individuals compensating for weak systems. When those individuals leave, risk surfaces immediately.
Compliance-First Architecture
Systems are designed to pass audits rather than to support safe execution, adaptability, or learning.
Fragmented Data
Clinical, operational, and financial data live in disconnected systems, preventing timely feedback and informed decisions.
Ungoverned Automation and AI
Automation is introduced without clear decision boundaries, escalation paths, or accountability when systems fail.
These patterns are systemic, not cultural. They persist even in high-performing organizations.
How Healthcare Organizations Reduce Execution Risk
Reducing execution risk in healthcare does not start with new tools. It starts with improving the systems that govern decisions.
Effective risk reduction focuses on:
- Clear decision ownership across clinical, operational, and technical domains
- Early feedback mechanisms that surface risk before commitments harden
- Incentives aligned with long-term stability rather than short-term output
- Escalation paths that function under real operational pressure
- Architectures that preserve optionality as regulations and care models evolve
The objective is not speed or perfection. The objective is resilient execution.
Why This Is Difficult to Do Internally
Healthcare organizations are optimized to deliver care, manage compliance, and control costs. They are rarely structured to step back and examine whether their decision systems themselves are creating risk.
External vendors are often incentivized to deliver artifacts: software, implementations, dashboards, or roadmaps. While valuable, these outputs rarely address the underlying execution dynamics that determine long-term outcomes.
CX.dev is structured differently. We are independently owned, with no incentives to maximize billable hours or create client dependency. Our work focuses on strengthening internal execution capability so organizations retain control over outcomes.
When Healthcare Leaders Engage CX.dev
Healthcare leaders typically reach out when:
- A platform or vendor decision feels locked in but outcomes are drifting
- A key individual is leaving and hidden risk becomes visible
- A digital health initiative delivers output without stability
- Regulatory pressure increases faster than system maturity
- AI or automation is introduced without governance or escalation clarity
These are not delivery problems. They are execution system problems.
Conclusion: Execution Risk Is Patient Risk
In healthcare, execution risk is not abstract. It compounds quietly and surfaces later through operational failure, regulatory exposure, and patient harm.
Reducing that risk requires better judgment, clearer decision systems, and incentives aligned with long-term value. That is where durable healthcare execution begins.
See Related Work
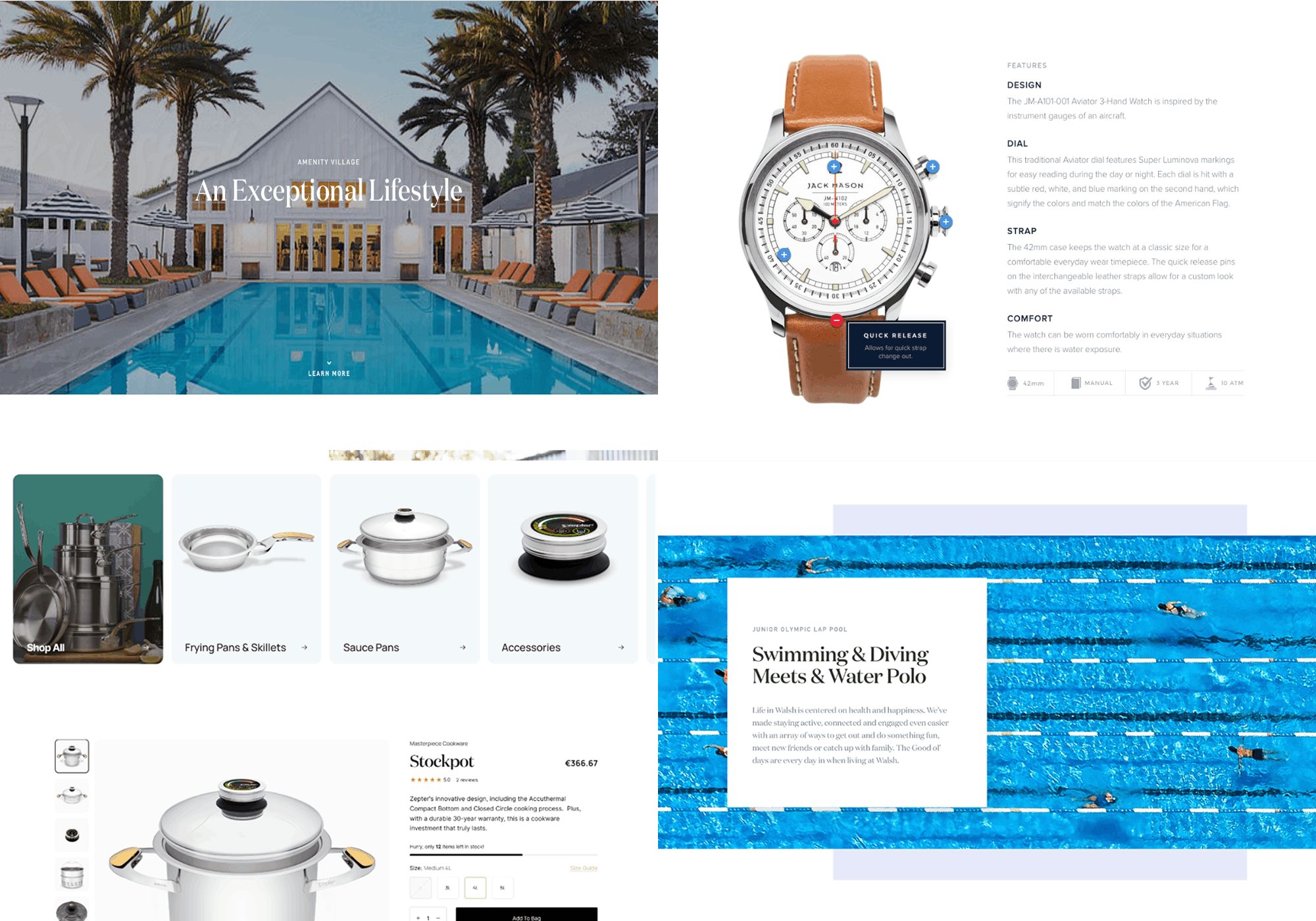
We'll show work that's relevant to the context and risks you're facing. We review together to ensure relevance and context.
Discuss Relevent Work